Process Management in Healthcare during the Covid-19 pandemic
Prof.dr Vojislav Stoiljković vojislav.stoiljkovic@cimlss.rs
Process Management in Healthcare during the Covid-19 pandemic
In “normal” times, the consequence of decisions on topics like operational efficiency, service stability, and ROI can break governments and change communities. In the case of a global pandemic, these issues become even more critical. Health systems in countries around the world are struggling; some are already overwhelmed. But within this gloomy prognosis, there is strong statistical evidence for deploying process management in global healthcare to improve patient wellbeing.[1]
At the forefront of COVID-19 are healthcare professionals who hold the lives of patients in their hands as they face possible serious consequences for their own health. Management of healthcare processes during COVID-19 can improve the treatment of patients, reduce the risk to the health of medical staff and reduce one of the unnecessary waste that occurs in all healthcare processes.[2]
The task of the manager, according to the famous guru Deming[3], is to ensure that everything that needs to be done is actually done and to prevent the occurrence of those events that should not happen. Harry Truman, for example, had a small sign on the table that read ” Responsibility cannot be placed on another.” This description is accurate because the manager is responsible for everything that happens in his jurisdiction
The inscription that the President of the United States had on his desk clearly indicates that the Crisis Headquarters cannot “transfer responsibility only to the citizens.” This means that the obligations and responsibilities of the Crisis Headquarters at the time of COVID-19 are such that it must ensure that everything that needs to be done to prevent the uncontrolled spread of the virus.
If we take a closer look at Deming’s opinion, we can expand his definition and ask the following question: “What are the essential responsibilities that the Crisis Headquarters cannot transfer to another? These responsibilities define the core managerial work of the Crisis Headquarters.”
This on the other hand indicates that the Crisis Headquarters can and should transfer part of the authority and responsibility in the fight against COVID-19 to lower levels all the way to the medical staff on the front line. In order for that staff to be able to accept responsibilities, they must have the opportunity and possibilities to acquaint the higher instance with the real state of affairs on the front line and to present their proposals. The higher instances should carefully consider this and, in open communication, accept some or all of the proposals and implement them in order to improve the management of the process of combating COVID-19. If this is not the case, then there is a huge waste in health care known as “INSUFFICIENT USE OF HUMAN POTENTIAL“. The potential and opinions of thousands of doctors and medical workers, who best see what happens in the process of treating patients infected with COVID-19, remain untapped, i.e. there is a large “WASTES“.
Health systems have one of the most complex infrastructures compared to other industries. Many processes intersect in the process of providing health care to patients. The functioning of such a system is complex, and it becomes especially critical during a pandemic. If health process management is ensured to function well, it is a finely tuned system that allows for the treatment and recovery of patients and provides faster services to families through social and administrative services.
The question is whether you can draw parallels with the automotive industry in complexity; a system in which complex processes absolutely must function or the whole process lags behind and is often shut down until the flow is restored. There is certainly no absolute parallel because there is no consistency in the influx of patients, the needs of each individual patient, and the like. However, there are approaches that can be used in healthcare processes, as pointed out by the great Deming in 14 points.
William Edwards Deming (October 14, 1900 – December 20, 1993)[4] established guiding principles that helped shape process management and forever changed the automotive industry.[5] Many of these principles can be applied here and help drive significant changes and improvements in the management of healthcare processes, especially during COVID-19
Point six of Deming’s principles is: “Establish on-the-job training.” Many physicians and medical personnel are encountering for the first time the use of respirators and other medical devices used to treat Covid-19 patients. They should be provided with timely and adequate on-the-job training in order to be able to use this equipment properly in providing medical care to patients.
The eighth point of Deming’s principles is: “Drive away fear so that everyone can work effectively (do the right thing) for the company.” In the health care system, this means driving away from the fear that doctors and medical staff will suffer. If there is fear among health professionals, the opportunity to hear and apply ideas and suggestions that could lead to a significant improvement in the COVID-19 response process will be missed. This will stifle the immeasurable resource and will not use the existing potential of health workers. Moreover, demoralized and fearful health workers will not be able to make the long-term contribution they would otherwise want and be able to make.
Improving the management of processes in health care refers to the management of the care process. Many managers in recent years have taken the wrong approach in trying to manage doctors, nurses, and other workers.
It is naive to think that process improvement begins and ends with pressure and threats on staff, at any level.
Frederick Winslow Taylor (March 20, 1856 – March 21, 1915)[6] was an American mechanical engineer striving to improve industrial efficiency. He is considered the father of scientific management. Frederick Taylor’s scientific theory of management, also called classical management theory, emphasizes efficiency, much like Max Weber. However, according to Taylor, instead of scolding employees for every minor mistake, employers should reward workers for increased productivity.
In one of his lectures, entitled “Success“, he wrote: “Every day, every year, every person should ask himself, once again and once again, two questions. First, “What is the name of the man I work for now? and, when he gets an unequivocal answer, then, “What does this man want me to do, right now?”
For Taylor, it didn’t matter, “What should I do in the interest of the company I work for?”.
This kind of management basically means listening to superiors and following their orders whether it is right or not. Figure 1 best illustrates this approach to management. The boss at the top is the smartest in everything. Beneath him are obedient who approve of all the decisions of the boss without thinking. At the lowest level are employees who should not think about anything but work as they are told. They are “headless” like “sheep”. The question is how can the “sheep” that are being led, as they were told, make a positive change and improve.
Figure 1 Taylor philosophy of management
Unfortunately, this approach is still present today, to a large extent, in the management of processes, and even in the management of the process of care and treatment of patients with Covid-19.
The new management applied by advanced companies, health care institutions, and society as a whole opens new questions: “What is the system for which I am responsible? Who are his customers? What do they require? How do customers define system output excellence? Do the people working in the system understand the definition of customer excellence? What do they see as obstacles to excellent performance? What can I do to change the system to remove these obstacles? How can they help me make and monitor change? What changes can we make that will go beyond that?”
A real manager knows that people have a brain and can use it. The task of the manager is to use the knowledge and potential of his associates to the greatest possible extent. This means that it should form teams to improve the process and thus allow all ideas and suggestions that can lead to progress to be heard (Figure 2).
Figure 2 Teams to improve the process of care and treatment of patients with Covid-19
Collaborators who can contribute the most to the improvement of the process are health workers on the front line who have a real insight into the situation, so they are in a position to propose adequate measures and changes in the process.
The tenth point of the principle reads: “Remove slogans, incentives, and goals for the workforce that require zero defects and new levels of productivity. Such incentives create only contradictory relationships because the majority of the causes of low quality and low productivity belong to the system and are therefore outside the workforce. “
The slogans of health workers are our heroes, they are the best fighters, we are grateful to them and they mean nothing. The root cause is poor management of processes that lead to increasing disruption, an increase in the number of infected, problems in care, more deaths, and ultimately to citizen dissatisfaction.
Better process and health management during Covid 19 starts with data.
“We believe in God, everything else must be shown by the data. ” In the case of the fight with COVID-19, it cannot be valid “I think vs the data already speaks for itself.“
In order to improve the management of the process, regardless of the process in health care in question, and especially the process that affects COVOD-19, the real numbers should be addressed. This is how the areas that need the most attention are assessed and found.
- Locations and micro-locations where there are the most positive ones
- What age structures are critical
- Where most time is wasted
- What causes the most delays in the adoption and implementation of measures
- Where are the shortcomings in communication
- How information is exchanged between departments, at the level of hospitals, clinical centers, according to the Crisis Staff, and especially how it is communicated to the public
- What is the response time of staff for urgent and non-urgent problems
- What are the patient satisfaction rates, how are they related to the processes
When dealing with a complex health system, process improvements must go up, sometimes through multiple levels of leadership, and even to the Crisis Staff and the Ministry of Health. The most effective way to make a change is to present data, real data. Fake data will then lead to a deterioration of management by the process of suppressing and preventing the spread of the corona. This will lead to mistrust and spread panic within health institutions and citizens.
It should include data showing current operational problems and efficiencies, while also showing some measures of performance data (even if predicted) that would come from improved process management.
The more people you add and the more data you change owners, the more complex and complicated the process becomes. This results in much slower processes and approvals. Much of the work is created as a result of failed or inefficient processes.
Use numbers to “sell” the need to improve and gain the trust of citizens, because the data can provide a huge insight into how more efficient processes will affect the overall situation, patient care, and communication among staff.
The ninth point in the 14 points of Deming[7], applied to Covid-19 reads: “Break down barriers in the management of the healthcare process during Covid 19.“
Break down barriers between ministries, clinical centers, hospitals, and doctors on the front lines in the fight against Corona 19. People in the Crisis Staff, directors of clinical centers, hospital directors and doctors and medical staff must work as a team to anticipate problems in caring for and treating patients from Covid-19”. If there are barriers then the voices of those health workers who are on the front line and who could contribute the most in the fight to Covi-19 are not heard.
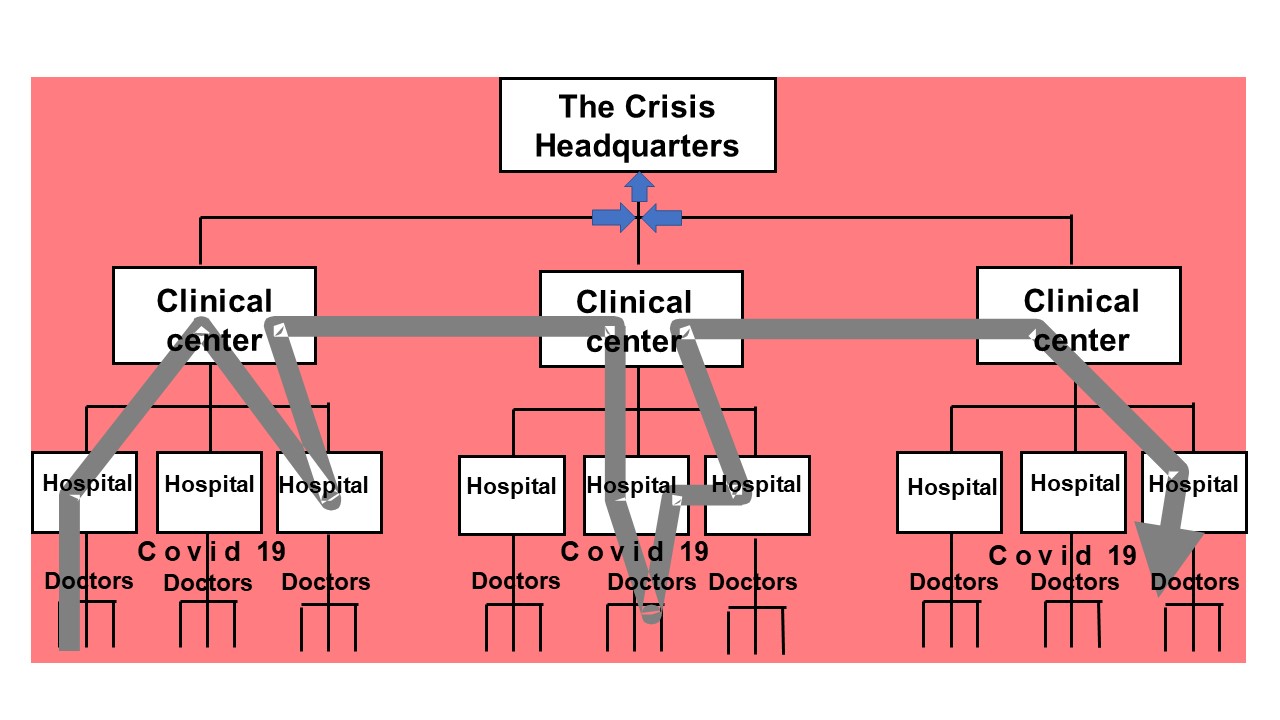
An illustration of the existence of a barrier in the existing management of the process of care and treatment of patients with Covid-19 is shown in Figure 3.
Figure 3 Barriers to communication
When there are barriers then the voice of doctors (health workers), who manage to pass it on to superiors, is first processed by superiors so that they can see if there is something in it that would be related to their responsibility. If they notice this, and this is the most common case, then they do not transfer the voice of the health workers to a higher new one or adjust it so that it seems as if everything is in the best order. The next level will act in the same way and in the end, the Crisis Headquarters, or whoever is at the top, will receive information that everything is “in the best order” and that no measures should be taken.
Even in a unified health care system, there are barriers between departments and administrations that can arise from personal, cultural, technological, and even geographical differences. Doctors and medical staff who directly provide care, directors, and everyone else up to the clerk, must work as a team. If that is not the case, the citizens and society will pay a high price.
When leadership can get their individual teams to work together with others, communication improves. It will also be possible to identify problems (and potential problems) in the processes that will ultimately lead to improvement.
“nvolve everyone in the health and ministry to work to achieve transformation. Healthcare transformation is everyone’s job.”[8]
In Nis, December 01, 2020. Prof.dr Vojislav Stoiljković
[1] https://www.signavio.com/post/process-management-in-global-healthcare/
[2] Vojislav Stoiljković, Lean in Healthcare, Lambert, 2018.
[3] https://deming.org/explore/fourteen-points/
[4] https://en.wikipedia.org/wiki/W._Edwards_Deming
[5] https://asq.org/quality-resources/total-quality-management/deming-points
[6] https://en.wikipedia.org/wiki/Frederick_Winslow_Taylor
[7] https://deming.org/explore/fourteen-points/
[8] Vojislav Stoiljković, Lean transformacija Srbije, Talija, 2018.